For patients 12 years of age and older with moderate to severe hidradenitis suppurativa (HS)
HUMIRA® (adalimumab) targets and blocks TNF-α to help address HS inflammation beneath the skin1-3
The relationship between these pharmacodynamic activities and the mechanism(s) by which HUMIRA exerts its clinical effects is unknown.
PIONEER I and II study design intro: PIONEER I (N=307) and II (N=326) were randomized, double-blind, placebo-controlled clinical trials in adult patients with moderate to severe HS receiving HUMIRA 40 mg weekly (after initial doses). Primary endpoint: HiSCR at Week 12 (Period A), defined as ≥50% reduction from baseline in abscess and inflammatory nodule count, with no increase in abscess count and draining tunnel count.4
HiSCR requires the following relative to baseline1,4:
Efficacy in adolescents extrapolated from adult data
HUMIRA efficacy in adolescent HS patients is extrapolated from the adult HS patient data based on the likelihood that the disease course and drug effects are similar to that of adults at the same exposure levels determined through pharmacokinetic modeling.1
HiSCR: response rates through OLE at Week 1686
OLE LIMITATIONS
In an open-label extension, there is a potential for enrichment of the long-term data in the remaining patient populations since patients who are unable to tolerate or do not respond to the drug often drop out.
EW=every week; EOW=every other week; HiSCR=Hidradenitis Suppurativa Clinical Response; LOCF=last observation carried forward; OLE=open-label extension.
Flares observed through Month 39
Integrated analysis of PIONEER I and PIONEER II through 12 weeks (Period A)
Flare: ≥25% increase in AN count and an absolute increase of ≥2 relative to baseline1,9
22% (of 100) patients who were withdrawn from HUMIRA after 12 weeks experienced flare.1
DATA LIMITATIONS
Flare and Days on Flare were pre-specified other secondary endpoints in Period A and not controlled for multiplicity. This data cannot be regarded as statistically or clinically significant, and therefore, no conclusions can be drawn.4,7
PIONEER I control=placebo
PIONEER II control=placebo +/- antibiotic
AN=abscess and inflammatory nodule; EW=every week; EOW=every other week; HiSCR=Hidradenitis Suppurativa Clinical Response;
OLE=open-label extension
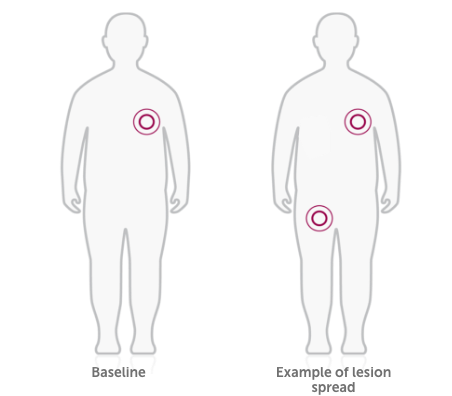
Lesion spread: integrated exploratory post hoc analysis of PIONEER I and II10
HUMIRA’s lesion spread data is an integrated exploratory post hoc analysis of PIONEER I and II. In the analysis, lesion spread was assessed through 36 weeks in patients randomized to HUMIRA 40 mg weekly or placebo in Periods A and B. PIONEER I and II are the only completed Phase 3 trials in HS.10
DATA LIMITATIONS
- Lesion spread was not a pre-specified endpoint and was not controlled for multiplicity. This data cannot be regarded as statistically or clinically significant, and therefore, no conclusions can be drawn.
- Placebo comparator is only available from PIONEER II, so differences should be interpreted with caution.
*HUMIRA 40 mg EW
EW=every week; EOW=every other week; HiSCR=Hidradenitis Suppurativa Clinical Response.
Safety: adverse events at Week 12 and Week 361,11
HS in adult patients
|
Serious AE |
Any AE leading |
Serious |
Malignancya,b |
Lymphoma |
Active |
||
PIONEER IAdverse events (AE) of Interest rates at Week 12 (Period A) |
HUMIRA |
8.6 |
2.9 |
2.9 |
0.0 |
0.0 |
0.0 |
|
Placebo |
20.2 |
8.7 |
0.0 |
2.9 |
0.0 |
0.0 |
||
PIONEER IIAdverse events (AE) of Interest rates at Week 36 (Periods A and B) |
HUMIRA |
14.0 |
8.7 |
3.5 |
0.0 |
0.0 |
0.0 |
|
Placebo |
30.0 |
17.7 |
5.4 |
0.0 |
0.0 |
0.0 |
||
aIn PIONEER I and II, malignancies excluded hepatosplenic T-cell lymphoma, leukemia, lymphoma, non-melanoma skin cancer, and melanoma.
bThe observed rate of lymphomas is approximately 0.11/100 PYs in clinical trials of HUMIRA-treated patients. This is approximately 3-fold higher than expected in the general population. Patients with RA and other chronic inflammatory diseases, particularly those with highly active disease and/or chronic exposure to immunosuppressant therapies, may be at a higher risk (up to several fold) than the general population for the development of lymphoma, even in the absence of TNF blockers.1
Safety: anticipated to be consistent in adolescents1
Safety of the recommended HUMIRA dose in the adolescent HS population is anticipated to be consistent with the known safety profile of HUMIRA based on a cross-indication safety profile of HUMIRA in both adults and pediatric patients at similar or higher exposure determined through pharmacokinetic modeling.
Safety: adverse events in the OLE period6,12
Adverse reaction rates observed in clinical trials may not predict the rates observed in a broader patient population in clinical practice.
|
Continuous HUMIRA EW Populationc |
Continuous HUMIRA EW Populationd |
||
Adverse Event |
n (%) |
Events (Events/100 PYs) |
n (%) |
Events (Events/100 PYs) |
Any serious AE |
12 (13.6) |
14 (7.2) |
58 (17.8) |
87 (13.3) |
Any AE leading to discontinuation of study drug |
13 (14.8) |
15 (7.7) |
51 (15.6) |
62 (9.5) |
Serious infection |
3 (3.4) |
3 (1.5) |
18 (5.5) |
20 (3.1) |
Any TB (active or latent) |
2 (2.3) |
2 (1.0) |
8 (2.5) |
8 (1.2) |
Any malignancy other than lymphoma, HSTCL, leukemia, NMSC, and melanoma |
0 |
0 |
3 (0.9) |
4 (0.6) |
Any lymphoma |
0 |
0 |
0 |
0 |
RISK OF MALIGNANCY1
Lymphoma, including a rare type of T-cell lymphoma, and other malignancies, some fatal, have been reported in patients treated with TNF blockers, including HUMIRA.
- More cases of malignancies were observed among HUMIRA-treated patients compared to control patients in clinical trials
- Consider the risks and benefits of HUMIRA treatment prior to initiating or continuing therapy in patients with a known malignancy
RISK OF TUBERCULOSIS1
Patients treated with HUMIRA are at increased risk for developing serious infections that may lead to hospitalization or death, including active tuberculosis (TB), which includes reactivation of latent TB. Patients with TB have frequently presented with disseminated or extrapulmonary disease.
- Test patients for latent TB before HUMIRA use and during therapy. Initiate treatment for latent TB prior to HUMIRA use
- Monitor patients closely for the development of signs and symptoms of infection during and after treatment with HUMIRA, including the development of TB in patients who tested negative for latent TB infection prior to initiating therapy
OLE LIMITATIONS
As with any long-term OLE there are several limitations with the OLE portion of this study. For example, there is potential for enrichment of the long-term data in the remaining patient population, as those who remain in the study generally fare better than those who discontinue.
HUMIRA has been studied for HS in 2 phase 3 controlled studies and 1 OLE study, and the safety profile for patients with HS treated with HUMIRA weekly dosing was consistent with the known safety profile of HUMIRA.
cStudy design dosing: HUMIRA EW/HUMIRA EW/HUMIRA EW.
dContinuous HUMIRA EW population consisted of those who were maintained on HUMIRA EW therapy once they started regardless of whether it was period A, B, or during the OLE (study design dosing: HUMIRA EW/EW/EW, CTRL/HUMIRA EW/HUMIRA EW, and Control/Control/HUMIRA EW populations).








 Lesions=abscesses, inflammatory nodules, or draining tunnels.
Lesions=abscesses, inflammatory nodules, or draining tunnels.
