For adult patients with moderate to severe Crohn’s disease (CD)
Remission and response in adult patients with CD1,*
CLASSIC-I
Anti-TNF-naïve patients with moderately to severely active Crohn's disease1
CLASSIC-I Study Design Intro: 4-week, randomized, double-blind, placebo-controlled study in 299 adults who have had conventional therapy. Patients were randomized to 1 of 4 treatment arms (± concomitant therapy). Primary endpoint: percentage of patients achieving induction of clinical remission* in the 2 higher doses vs control at Week 4.1,2
*Clinical remission was defined as a Crohn's Disease Activity Index (CDAI) score <150 points.2
Remission* and response†: Week 4
Remission for Total Population at Week 4 (Primary Endpoint)
All Patients Were Bio-naïve1,2
- HUMIRA 160 mg/80 mg (n=76)
- Placebo (n=74)
Response for Total Population at Week 4 (Secondary Endpoint)
All Patients Were Bio-naïve1,2
- HUMIRA 160 mg/80 mg (n=76)
- Placebo (n=74)
aP=0.001 HUMIRA vs placebo
bP=0.007 HUMIRA vs placebo
*Clinical remission was defined as a Crohn’s Disease Activity Index (CDAI) score <150 points.
†Clinical response (CR-70; symptom improvement) was defined as a reduction of ≥70 points from baseline CDAI score.
CHARM
Adult patients with moderately to severely active Crohn's disease1
CHARM Study Design Intro: 56-week, randomized controlled study in 854 adults. All patients received open-label HUMIRA 80 mg at Week 0 and 40 mg at Week 2. The 499 patients with CR-70 response at Week 4 were randomized to one of three treatment arms (± concomitant conventional therapy) and were included in the analysis. Co-primary endpoints: Clinical remission (Week 26, Week 56) for each HUMIRA group vs control in the 499 patients with CR-70 response at Week 4.1,3
Remission*: total population at Weeks 26 and 56 (co-primary endpoints)1,3
~50% of Patients Were Bio-naïve and ~50% of Patients Were Bio-experienced3
Double-blind, placebo-controlled period
Week 26
- HUMIRA 40 mg EOW (n=68/172)
- Control (n=29/170)
Week 56
- HUMIRA 40 mg EOW (n=62/172)
- Control (n=20/170)
aP<0.001, HUMIRA vs control.
*Clinical remission was defined as a Crohn’s Disease Activity Index score <150 points.
EOW=every other week
Remission*: corticosteroid-free patients at Weeks 26 and 563
Patients steroid-free for ≥90 days
Week 26
Nonranked Secondary Endpoint
- HUMIRA 40 mg EOW (n=11/58)
- Control (n=2/66)
Week 56
Ranked Secondary Endpoint
- HUMIRA 40 mg EOW (n=17/58)
- Control (n=3/66)
DATA LIMITATIONS
This analysis is not powered or tested to demonstrate a statistically significant difference in treatment effect; no statistical inferences can be made due to the exploratory nature of the analysis and should be cautiously interpreted.
aP<0.001, HUMIRA vs control.
*Clinical remission was defined as a Crohn’s Disease Activity Index score <150 points.
Response*: total population at Weeks 26 and 56 (prespecified secondary endpoints)1,3
~50% of Patients Were Bio-naïve and ~50% of Patients Were Bio-experienced1,4
Double-blind, placebo-controlled period
Week 26
- HUMIRA 40 mg EOW (n=93/172)
- Control (n=48/170)
Week 56
- HUMIRA 40 mg EOW (n=74/172)
- Control (n=30/170)
aP<0.001, HUMIRA vs control.
*Clinical response (CR-70; symptom improvement) was defined as a reduction of ≥70 points from baseline Crohn’s Disease Activity Index score.
EOW=every other week
Long-term remission*: 4 years1,4
Among patients not in response† by Week 12, continued therapy did not result in significantly more responses.
CHARM RCT (56 weeks)
- HUMIRA 40 mg EOW (n=172)
- Control
CHARM OLE Observed Analysis (156 weeks)
- % of patients in remission (HUMIRA 40 mg EOW)
aP<0.001
*Clinical remission was defined as a CDAI score <150 points.
†Clinical response (CR-70; symptom improvement) was defined as a reduction of ≥70 points from baseline CDAI score.
The use of HUMIRA in CD beyond 1 year has not been evaluated in controlled clinical studies.
- OLE populations generally consist of treatment responders, as patients who are unable to tolerate the drug or who do not respond to the drug drop out.
- Patients who dropped out of the OLE trial or who were missing Crohn’s Disease Activity Index (CDAI) scores were not included in the analysis at each time point.4
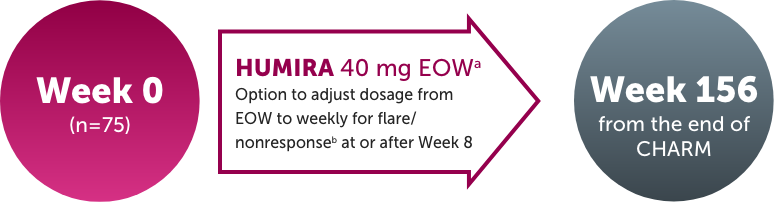
OLE Study Design Intro: This subanalysis includes patients from the CHARM trial who were randomized responders, remained blinded on HUMIRA 40 mg EOW therapy for the duration of the trial, and entered (N=75) and remained on HUMIRA 40 mg EOW in the OLE.4
EOW=every other week; OLE=open-label extension; RCT=randomized controlled trial
Safety data: 5 years5
Adverse reaction rates observed in clinical trials and OLE studies may not predict the rates observed in a broader patient population in clinical practice.
Rates (events per 100 PYs) of treatment-emergent adverse events (AEs)* of interest in 9 controlled and uncontrolled moderate to severe adult CD studies✝ for:
Risk of Serious Infection

Patients treated with HUMIRA are at increased risk for developing serious infections that may lead to hospitalization or death. Most patients who developed these infections were taking concomitant immunosuppressants such as methotrexate or corticosteroids.1
Carefully consider the risks and benefits of treatment with HUMIRA prior to initiating therapy in patients with chronic or recurrent infection. Monitor patients closely for the development of signs and symptoms of infection during and after treatment with HUMIRA.1
- Do not start HUMIRA in patients with an active infection, including localized infections.
- Patients older than 65 years, patients with co-morbid conditions, and/or patients taking concomitant immunosuppressants may be at greater risk of infection.
The use of HUMIRA in CD beyond 1 year has not been evaluated in controlled clinical studies.
- OLE populations generally consist of treatment responders, as patients who are unable to tolerate the drug or who do not respond to the drug drop out.
CHARM Study Design Intro: 56-week, randomized controlled study in 854 adults. All patients received open-label HUMIRA 80 mg at Week 0 and 40 mg at Week 2. The 499 patients with CR-70 response at Week 4 were randomized to one of three treatment arms (± concomitant conventional therapy) and were included in the analysis.1,3
aData as of December 31, 2014.
bNine pooled controlled and uncontrolled studies.
cControl=placebo ± concomitant therapy.
*Treatment-emergent AE is defined as any adverse event with an onset date on or after the first HUMIRA dose and up to 70 days after the last dose of HUMIRA.
✝Excluding Japanese studies.
EOW=every other week; OLE=open-label extension; PYs=patient-years; RCT=randomized controlled trial
Risk of Tuberculosis

Patients treated with HUMIRA are at increased risk for developing serious infections that may lead to hospitalization or death, including active tuberculosis (TB), including reactivation of latent TB. Patients with TB have frequently presented with disseminated or extrapulmonary disease.1
- Test patients for latent TB before HUMIRA use and during therapy. Initiate treatment for latent TB prior to HUMIRA use.
- Monitor patients closely for the development of signs and symptoms of infection during and after treatment with HUMIRA, including the development of TB in patients who tested negative for latent TB infection prior to initiating therapy.
The use of HUMIRA in CD beyond 1 year has not been evaluated in controlled clinical studies.
- OLE populations generally consist of treatment responders, as patients who are unable to tolerate the drug or who do not respond to the drug drop out.
CHARM Study Design Intro: 56-week, randomized controlled study in 854 adults. All patients received open-label HUMIRA 80 mg at Week 0 and 40 mg at Week 2. The 499 patients with CR-70 response at Week 4 were randomized to one of three treatment arms (± concomitant conventional therapy) and were included in the analysis.1,3
aData as of December 31, 2014.
bNine pooled controlled and uncontrolled studies.
cControl=placebo ± concomitant therapy.
*Treatment-emergent AE is defined as any adverse event with an onset date on or after the first HUMIRA dose and up to 70 days after the last dose of HUMIRA.
✝Excluding Japanese studies.
EOW=every other week; OLE=open-label extension; PYs=patient-years; RCT=randomized controlled trial
Risk of Malignancya

Lymphoma, including a rare type of T-cell lymphoma, and other malignancies, some fatal, have been reported in patients treated with TNF blockers, including HUMIRA.1
- Carefully consider the risks and benefits of treatment with HUMIRA prior to initiating therapy in patients with a known malignancy.
- More cases of malignancies were observed among HUMIRA-treated patients compared to control patients in clinical trials.
Risk of HSTCL1
Postmarketing cases of hepatosplenic T-cell lymphoma (HSTCL), a rare type of fatal lymphoma, have been reported in patients treated with TNF blockers including HUMIRA. The majority of cases were in adolescent and young adult males with inflammatory bowel disease who had received concomitant or prior treatment with azathioprine or 6-mercaptopurine.
The use of HUMIRA in CD beyond 1 year has not been evaluated in controlled clinical studies.
- OLE populations generally consist of treatment responders, as patients who are unable to tolerate the drug or who do not respond to the drug drop out.
CHARM Study Design Intro: 56-week, randomized controlled study in 854 adults. All patients received open-label HUMIRA 80 mg at Week 0 and 40 mg at Week 2. The 499 patients with CR-70 response at Week 4 were randomized to one of three treatment arms (± concomitant conventional therapy) and were included in the analysis.1,3
aExcluding non-melanoma skin cancer and lymphoma.
bData as of December 31, 2014.
cNine pooled controlled and uncontrolled studies.
dControl=placebo ± concomitant therapy.
*Treatment-emergent AE is defined as any adverse event with an onset date on or after the first HUMIRA dose and up to 70 days after the last dose of HUMIRA.
✝Excluding Japanese studies.
EOW=every other week; OLE=open-label extension; PYs=patient-years; RCT=randomized controlled trial
Risk of Lymphoma

Lymphoma and other malignancies, some fatal, have been reported in children and adolescent patients treated with TNF blockers, of which HUMIRA is a member.1
Postmarketing cases of hepatosplenic T-cell lymphoma (HSTCL), a rare type of T-cell lymphoma, have occurred in adolescent and young adults with inflammatory bowel disease treated with TNF blockers including HUMIRA.1
The rate of lymphoma in controlled and uncontrolled clinical trials of HUMIRA was approximately 3-fold higher than expected in the general population.1
Patients with chronic inflammatory diseases, particularly those with highly active disease, are at a higher risk for the development of lymphoma.1
The use of HUMIRA in CD beyond 1 year has not been evaluated in controlled clinical studies.
- OLE populations generally consist of treatment responders, as patients who are unable to tolerate the drug or who do not respond to the drug drop out.
CHARM Study Design Intro: 56-week, randomized controlled study in 854 adults. All patients received open-label HUMIRA 80 mg at Week 0 and 40 mg at Week 2. The 499 patients with CR-70 response at Week 4 were randomized to one of three treatment arms (± concomitant conventional therapy) and were included in the analysis.1,3
aData as of December 31, 2014.
bNine pooled controlled and uncontrolled studies..
cControl=placebo ± concomitant therapy.
*Treatment-emergent AE is defined as any adverse event with an onset date on or after the first HUMIRA dose and up to 70 days after the last dose of HUMIRA.
✝Excluding Japanese studies.
EOW=every other week; OLE=open-label extension; PYs=patient-years; RCT=randomized controlled trial
PYRAMID registry7
A prospective postmarketing registry assessing HUMIRA safety in routine clinical practice
Study Design Intro: PYRAMID was a multicenter, uncontrolled, observational registry of 5025 (16680.4 PYs) adult patients with moderately to severely active CD treated with HUMIRA in a routine clinical practice setting. Patients were newly prescribed or currently receiving HUMIRA according to local product labels and were followed for up to 6 years. The mean HUMIRA exposure was over 3 years. The primary goal was to rule out a doubling of the risk of lymphoma in patients treated with HUMIRA from an estimated background lymphoma rate in the general population adjusted for thiopurine use.
PYs=patient-years; TNF=tumor necrosis factor
Safety Considerations1
Serious Infections
Patients treated with HUMIRA are at increased risk for developing serious infections that may lead to hospitalization or death. These infections include active tuberculosis (TB), reactivation of latent TB, invasive fungal infections, and bacterial, viral, and other infections due to opportunistic pathogens. Most patients who developed these infections were taking concomitant immunosuppressants such as methotrexate or corticosteroids.
Malignancies
Lymphoma, including a rare type of T-cell lymphoma, and other malignancies, some fatal, have been reported in patients treated with TNF blockers, including HUMIRA.
Other Serious Adverse Reactions
Patients treated with HUMIRA also may be at risk for other serious adverse reactions, including anaphylaxis, hepatitis B virus reactivation, demyelinating disease, cytopenias, pancytopenia, heart failure, and a lupus-like syndrome.
Risk of HSTCL
Postmarketing cases of hepatosplenic T-cell lymphoma (HSTCL), a rare type of fatal lymphoma, have been reported in patients treated with TNF blockers, including HUMIRA. The majority of cases were in adolescent and young adult males with inflammatory bowel disease who had received concomitant or prior treatment with azathioprine or 6-mercaptopurine.
Summary of registry treatment-emergent adverse events (AEs)7
| Adverse Events | HUMIRA N=5025 (n) |
HUMIRA PYs=16680.4, Events (E/100 PY) |
| Any AE | 47.6% (2392) | 6124 (36.7) |
| Serious AE | 36.9% (1853) | 4129 (24.8) |
| Serious AE at least possibly related to HUMIRAa | 8.4% (422) | 627 (3.8) |
| AE leading to HUMIRA discontinuation | 11.9% (596) | 766 (4.6) |
| AE leading to death | 0.9% (43) | 52 (0.3) |
| Any infection | 17.0% (855) | 1333 (8.0) |
| Serious infection | 11.1% (556) | 792 (4.7) |
| Opportunistic infection (excluding oral candidiasis and TB) | 0.4% (19) | 21 (0.1) |
| Active TB | 0.2% (10) | 10 (<0.1) |
| Latent TB | 0.1% (7) | 7 (<0.1) |
| Any malignancy | 2.3% (116) | 134 (0.8) |
| NMSC | 0.7% (36) | 49 (0.3) |
| Lymphoma | 0.2% (10) | 10 (0.06) |
| Melanoma | 0.2% (11) | 12 (<0.1) |
| Leukemia | <0.1% (3) | 3 (<0.1) |
| Malignancy other than lymphoma, leukemia, NMSC, or melanoma | 1.2% (60) | 60 (0.4) |
| Injection site reaction | 0.2% (12) | 22 (0.1) |
| Demyelinating disorder | 0.2% (8) | 8 (<0.1) |
DATA LIMITATIONS
- Observational data are subject to outcome-reporting bias and the bias related to rules attributing safety events to HUMIRA despite exposure to other therapies and results should be cautiously interpreted.
Safety profile consistent with known safety profile from global clinical trials and across approved indications7
- Rate of infections consistent with previously reported infection rates in clinical trials of HUMIRA and other anti-TNF agents.
- Malignancy and lymphoma rates did not exceed estimated rates based upon the general population.
- Malignancy rates in HUMIRA-treated patients consistent with previously reported malignancy rates in clinical trials of HUMIRA for multiple indications and similar rates were observed for anti-TNF agents.
- No increase in the relative risk of non-melanoma skin cancer or other malignancies in patients receiving HUMIRA monotherapy. In contrast, patients treated with HUMIRA plus immunomodulator had significantly increased risks of malignancies compared with the general population.
aAs assessed by investigator.
NMSC=non-melanoma skin cancer; PYs=patient-years; TB=tuberculosis